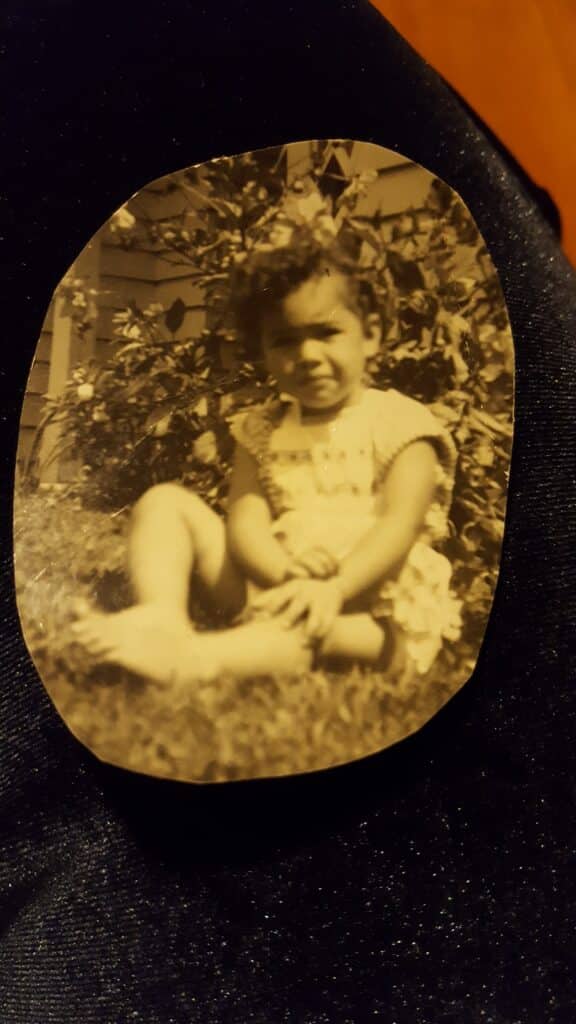
After being diagnosed with breast cancer in 2021, at age 60, Ali Coomber–a Samoan woman living in New Zealand– describes her initial thoughts as “quite scattered” as she felt like she was existing “in a world of unreality”.
Coming up to two years now since her double mastectomy, Coomber looks back and remembers the many conflicting thoughts and emotions that she experienced throughout the journey.
“Part of me was very emotional, another part said I could get through this, and yet another part said it will be what it will be,” she says. “I kept thinking about getting my affairs in order, what I had to do and who I wanted to say goodbye to, and what different people meant to me.”

While breast cancer is the most commonly diagnosed cancer for women, those from Māori, Pasifika and Indigenous Australian communities experience higher breast cancer mortality, lower breast screening rates and are under-represented in clinical trials research.
With breast cancer already being a life-altering diagnosis, it can cause even more stress for members of the Māori, Pasifika and Indigenous Australian communities to know that these medical disparities exist.

Coomber says seeing the statistics released earlier this year from the report 30,000 Voices: Informing a Better Future for Breast Cancer in New Zealand, made her “highly concerned for Pasifika women” and “wanting to support in any way possible”.
Pasifika women are 52 per cent more likely and Wàhine Māori are 33 per cent more likely to die of breast cancer within 10 years of diagnosis, compared with Pàkehà (European ancestry) women.
In addition, Wàhine Māori were more likely to have higher-risk HER2-positive breast cancer than European women. Pasifika women also have the highest rates of life-threatening stage 3 and 4 breast cancer and of HER2-positive cancers, as well as more fast-growing grade 3 tumours than all other ethnicities.
“Being Samoan and seeing these figures makes me enormously uneasy,” says Coomber.
“I sometimes wonder if I will even make it to 5 years, which is unnerving– however, I continue to go about life as optimistic as I can be.”

Since starting her breast cancer treatment, Coomber has learned a lot and would advise other Pasifika women to handle their diagnosis in the way that best suits them “at any given time”.
“Understand it can be a very emotional time, and this is okay,” she says. “Have really good family or friends around you. Talk, cry and laugh.”

During treatment, Coomber also kept a notebook with her to write down even the smallest of questions as she says “having knowledge is empowering”.
“Pasifika people can be shy when asking questions, I have struck this on occasion with family members in medical situations,” she says. “Don’t be shy, we count.”

Disparities in breast cancer treatment are prevalent in Australia as well.
Although Aboriginal women are 0.9 times as likely to be diagnosed with breast cancer, they are 1.2 times more likely to die from breast cancer than the wider population.
The five-year survival rate for Aboriginal women with breast cancer is also lower at 81 per cent compared to the general population of 92 per cent.
And breast screening rates for Aboriginal women are lower compared to non-Indigenous Australians, at 37.3 per cent vs. 53.2 per cent.
Having worked with Māori, Pasifika and Indigenous Australian breast cancer patients, Associate Professor Andrew Redfern says he’s observed “that Aboriginal women are more likely to prioritise family over themselves and sometimes choose not to have treatment or delay treatment because of the need to care for younger generations or help their children.”
Dr Redfern is an Associate Professor of Medical Oncology at the University of Western Australia, Associate Director for Clinical Strategy at Harry Perkins Institute of Medical Research, Consultant Medical Oncologist at the Fiona Stanley Hospital, Perth, and Medical Director of Linear Clinical Research specialising in early phase human trials.
Through his research, he’s found that Indigenous women with breast cancer have a death rate about three and a half times higher than non-Indigenous women with breast cancer.
“We’ve seen a lot of other differences [as well],” says Dr. Redfern, noting that while the Indigenous and non-Indigenous women they studied were given chemotherapy and radiation therapy at the same rate, the Indigenous population was given less intensive treatment.
Moving forwards from these findings, he says one of the things his team is doing is “looking at identifying Aboriginal women as they’re diagnosed with breast cancer and then discussing their cases with their local treatment team and their Aboriginal health care workers.”
With the research showing an urgent need for change, Dr Redfern says this work will include Indigenous representation and cultural geographical input as it aims to put patients first.
Join Breast Cancer Trials’ next free and online Q&A, happening Wednesday 26 July. The session will be on the topic of breast cancer in the Indigenous, Māori and Pasifika communities. To register, click here.

